Ferroptosis-centered Drug Response Information
General Information of the Drug (ID: ferrodrug0176)
| Name |
Baicalin
|
||||
|---|---|---|---|---|---|
| Synonyms |
Baicalin; 21967-41-9; Baicalein 7-O-glucuronide; 7-D-Glucuronic acid-5,6-dihydroxyflavone; CHEBI:2981; Baicalein 7-glucuronide; MFCD00134418; 347Q89U4M5; 5,6-dihydroxy-4-oxo-2-phenyl-4H-chromen-7-yl beta-D-glucopyranosiduronic acid; CHEMBL485818; UNII-347Q89U4M5; 5,6,7-trihydroxyflavone 7-O-beta-D-glucuronide; Baicalein 7-O-.beta.-D-glucuronide; (2S,3S,4S,5R,6S)-6-[(5,6-dihydroxy-4-oxo-2-phenyl-4H-chromen-7-yl)oxy]-3,4,5-trihydroxyoxane-2-carboxylic acid; beta-D-Glucopyranosiduronic acid, 5,6-dihydroxy-4-oxo-2-phenyl-4H-1-benzopyran-7-yl; 5,6-dihydroxy-4-oxo-2-phenyl-4H-1-benzopyran-7-yl beta-D-glucopyranosiduronic acid; 5,6-Dihydroxy-4-oxo-2-phenyl-4H-1-benzopyran-7-yl ; A-D-Glucopyranosiduronic Acid; BAICALEIN 7-O-GLUCURONIDE (USP-RS); BAICALEIN 7-O-GLUCURONIDE [USP-RS]; BAICALEIN 7-O-BETA-D-GLUCURONIDE; baikalin; Baicaloside; 31564-28-0; Baicalin,(S); (2S,3S,4S,5R,6S)-6-(5,6-dihydroxy-4-oxo-2-phenyl-4H-chromen-7-yloxy)-3,4,5-trihydroxytetrahydro-2H-pyran-2-carboxylic acid; 0XE; Baicalin, 95%; (2S,3S,4S,5R,6S)-6-((5,6-dihydroxy-4-oxo-2-phenyl-4H-chromen-7-yl)oxy)-3,4,5-trihydroxytetrahydro-2H-pyran-2-carboxylic acid; BAICALIN [INCI]; 7-D-glucuronic acid-5,6-dihydroxy-flavone; BAICALIN [VANDF]; Baicalein-7-D-glucuronide; BAICALIN [WHO-DD]; SCHEMBL285082; Baicalein 7-beta-D-glucuronide; Baicalein 7-O-b-D-glucuronide; TJN-151; IKIIZLYTISPENI-ZFORQUDYSA-N; DTXSID701346569; Baicalin, >=99.0% (HPLC); HY-N0197; BDBM50242173; AKOS007930529; AKOS015955933; Baicalin 1000 microg/mL in Methanol; AC-7990; AM84780; CCG-214128; CS-5302; Baicalein 7-beta-D-glucopyranosiduronate; NCGC00386028-03; (2S,3S,4S,5R,6S)-6-(5,6-DIHYDROXY-4-OXO-2-PHENYL-CHROMEN-7-YL)OXY-3,4,5-TRIHYDROXY-OXANE-2-CARBOXYLIC ACID; (2S,3S,4S,5R,6S)-6-(5,6-dihydroxy-4-oxo-2-phenyl-chromen-7-yl)oxy-3,4,5-trihydroxy-tetrahydropyran-2-carboxylic acid; AS-13226; PD132941; A815791; J-013512; Q-100275; Q2879368; BRD-K49962337-001-01-1; Baicalin, European Pharmacopoeia (EP) Reference Standard; 5,6,7-Trihydroxyflavone-7-O-.beta.-D-glucopyranosideuronic acid; (2S,3S,4S,5R,6R)-6-(5,6-dihydroxy-4-oxo-2-phenyl-chromen-7-yl)oxy-3,4,5-trihydroxy-tetrahydropyran-2-carboxylic acid; (2S,3S,4S,5R,6S)-6-(5,6-dihydroxy-4-oxo-2-phenyl-4H-chromen-7-yloxy)-3,4,5-trihydroxy-tetrahydro-2H-pyran-2-carboxylic acid; (2S,3S,4S,5R,6S)-6-(5,6-dihydroxy-4-oxo-2-phenylchromen-7-yl)oxy-3,4,5-trihydroxyoxane-2-carboxylicacid; .BETA.-D-GLUCOPYRANOSIDURONIC ACID, 5,6-DIHYDROXY-4-OXO-2-PHENYL-4H-1-BENZOPYRAN-7-YL
Click to Show/Hide
|
||||
| Status |
Terminated
|
||||
| Drug Type |
Small molecular drug
|
||||
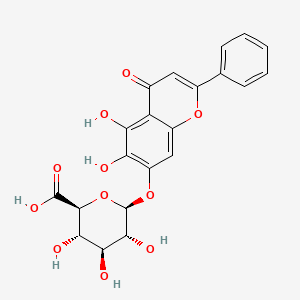
| Structure |
 |
||||
| Formula |
C21H18O11
|
||||
| IUPAC Name |
(2S,3S,4S,5R,6S)-6-(5,6-dihydroxy-4-oxo-2-phenylchromen-7-yl)oxy-3,4,5-trihydroxyoxane-2-carboxylic acid
|
||||
| Canonical SMILES |
C1=CC=C(C=C1)C2=CC(=O)C3=C(C(=C(C=C3O2)OC4C(C(C(C(O4)C(=O)O)O)O)O)O)O
|
||||
| InChI |
InChI=1S/C21H18O11/c22-9-6-10(8-4-2-1-3-5-8)30-11-7-12(14(23)15(24)13(9)11)31-21-18(27)16(25)17(26)19(32-21)20(28)29/h1-7,16-19,21,23-27H,(H,28,29)/t16-,17-,18+,19-,21+/m0/s1
|
||||
| InChIKey |
IKIIZLYTISPENI-ZFORQUDYSA-N
|
||||
| PubChem CID | |||||
| TTD Drug ID | |||||
Full List of Ferroptosis Target Related to This Drug
Nuclear factor erythroid 2-related factor 2 (NFE2L2)
| In total 3 item(s) under this Target | |||||
| Experiment 1 Reporting the Ferroptosis-centered Drug Act on This Target | [1] | ||||
| Target for Ferroptosis | Marker/Suppressor | ||||
| Responsed Disease | Injury of intra-abdominal organs | ICD-11: NB91 | |||
| Responsed Regulator | Kelch-like ECH-associated protein 1 (KEAP1) | Driver | |||
| Pathway Response | Pathways in cancer | hsa05200 | |||
| Ferroptosis | hsa04216 | ||||
| Cell Process | Cell ferroptosis | ||||
| In Vivo Model |
C57BL/6 mice at 6-8 weeks were intraperitoneally injected with D-GalN/LPS (1772-03-8/L2880, Sigma-Aldrich, USA) at a dose of 700 mg/kg and 10 ug/kg, respectively. The constructed D-GaIN/LPS-induced ALI model mice were named the model group, and the normal mice injected with phosphate-buffered saline (PBS) were named the blank group. After 1 h of LPS/D-GalN treatment, Exo and Ba-Exo (150 ug/mice) were injected into the tail vein of the mice in the Exo and Ba-Exo groups, respectively. Mice were sacrificed via anesthesia overdose 12 h after the intervention. Half of the liver tissue was fixed in paraformaldehyde, while the other half was frozen at 80 . Peripheral blood serum was stored at -80 .
Click to Show/Hide
|
||||
| Response regulation | Baicalin-pretreated MSCs (Ba-Exo) exerts a protective effect on liver function and activates the Keap1-NRF2 pathway via P62 (SQSTM1), thereby inhibiting ROS production and lipid peroxide-induced ferroptosis. Therefore, baicalin pretreatment is an effective and promising approach in optimizing the therapeutic efficacy of Exo in acute liver injury (ALI). | ||||
| Experiment 2 Reporting the Ferroptosis-centered Drug Act on This Target | [1] | ||||
| Target for Ferroptosis | Marker/Suppressor | ||||
| Responsed Disease | Injury of intra-abdominal organs | ICD-11: NB91 | |||
| Responsed Regulator | Sequestosome-1 (SQSTM1) | Driver | |||
| Pathway Response | Pathways in cancer | hsa05200 | |||
| Ferroptosis | hsa04216 | ||||
| Cell Process | Cell ferroptosis | ||||
| In Vivo Model |
C57BL/6 mice at 6-8 weeks were intraperitoneally injected with D-GalN/LPS (1772-03-8/L2880, Sigma-Aldrich, USA) at a dose of 700 mg/kg and 10 ug/kg, respectively. The constructed D-GaIN/LPS-induced ALI model mice were named the model group, and the normal mice injected with phosphate-buffered saline (PBS) were named the blank group. After 1 h of LPS/D-GalN treatment, Exo and Ba-Exo (150 ug/mice) were injected into the tail vein of the mice in the Exo and Ba-Exo groups, respectively. Mice were sacrificed via anesthesia overdose 12 h after the intervention. Half of the liver tissue was fixed in paraformaldehyde, while the other half was frozen at 80 . Peripheral blood serum was stored at -80 .
Click to Show/Hide
|
||||
| Response regulation | Baicalin-pretreated MSCs (Ba-Exo) exerts a protective effect on liver function and activates the Keap1-NRF2 pathway via P62 (SQSTM1), thereby inhibiting ROS production and lipid peroxide-induced ferroptosis. Therefore, baicalin pretreatment is an effective and promising approach in optimizing the therapeutic efficacy of Exo in acute liver injury (ALI). | ||||
| Experiment 3 Reporting the Ferroptosis-centered Drug Act on This Target | [3] | ||||
| Target for Ferroptosis | Marker/Suppressor | ||||
| Responsed Disease | Osteosarcoma | ICD-11: 2B51 | |||
| Pathway Response | Ferroptosis | hsa04216 | |||
| Cell Process | Cell ferroptosis | ||||
| In Vitro Model | MG-63 cells | Osteosarcoma | Homo sapiens | CVCL_0426 | |
| 143B cells | Osteosarcoma | Homo sapiens | CVCL_2270 | ||
| hBMMSCs (Human bone marrow mesenchymal stem cells) | |||||
| In Vivo Model |
A total of 24 BALB/c-nude mice (4-5 weeks old) were purchased and MG63 cells were injected into the right tibial bone marrow cavity of mice in a volume of 1 x 106/100 ul. When the tumor volume was visible, all animals were randomly divided into four groups (n = 6): the control (10% DMSO + 40% PEG300 + 5% Tween-80 + 45% Saline) group, the baicalin (200 mg/kg/day) group, the Fer-1 (0.8 mg/kg/day) group and Fer-1 + baicalin group. The baicalin and Fer-1 were intraperitoneally administered every day for two consecutive weeks and tumor sizes were measured every two days.
Click to Show/Hide
|
||||
| Response regulation | By promoting the Fe accumulation, ROS formation, MDA production and suppressing the ratio of GSH/GSSG, baicalin was found to trigger ferroptosis in Osteosarcoma and ferroptosis inhibitor ferrostatin-1 (Fer-1) successfully reversed these suppressive effects, indicating that ferroptosis participated in the baicalin mediated anti-OS activity. Mechanistically, baicalin physically interacted with Nrf2, a critical regulator of ferroptosis, and influenced its stability via inducing ubiquitin degradation, which suppressed the Nrf2 downstream targets GPX4 and xCT expression, and led to stimulating ferroptosis. | ||||
Unspecific Target
| In total 2 item(s) under this Target | |||||
| Experiment 1 Reporting the Ferroptosis-centered Drug Act on This Target | [2] | ||||
| Responsed Disease | Traumatic brain injury | ICD-11: NA07 | |||
| Responsed Regulator | Microtubule-associated proteins 1A/1B light chain 3A (MAP1LC3A) | Driver | |||
| Pathway Response | Ferroptosis | hsa04216 | |||
| Cell Process | Cell ferroptosis | ||||
| Cell autophagy | |||||
| Cell apoptosis | |||||
| In Vitro Model | rPNs (Rat primary neurons) | ||||
| In Vivo Model |
Rats were injected with 4 mL/kg of chloral hydrate for anesthesia and then put on a stereotactic apparatus. Subsequently, the needle was tilted at 55 in the sagittal plane and fixed anterior to the bregma (7.5 mm). The needle tip was toward the right and lowered the anterior to the chiasma (2 mm). Finally, the nonheparinized autologous femoral arterial blood (0.3 mL) was injected into a prechiasmatic cistern using a syringe pump. Rat temperature was maintained at 37 ± 0.5 during the surgery. The rats in the sham group were injected with the same dose of saline into a prechiasmatic cistern. At last, rats were monitored for recovery and then returned to cages.
Click to Show/Hide
|
||||
| Response regulation | Baicalin was confirmed to suppress the beclin1, LC3-II, and LC3-I protein levels in rat brain tissues. Moreover, we found that baicalin inhibited neuronal apoptosis. Overall, baicalin suppressed autophagy-dependent ferroptosis in early brain injury after subarachnoid hemorrhage. | ||||
| Experiment 2 Reporting the Ferroptosis-centered Drug Act on This Target | [2] | ||||
| Responsed Disease | Traumatic brain injury | ICD-11: NA07 | |||
| Responsed Regulator | Microtubule-associated proteins 1A/1B light chain 3B {ECO:0000305} (MAP1LC3B) | Driver | |||
| Pathway Response | Ferroptosis | hsa04216 | |||
| Cell Process | Cell ferroptosis | ||||
| Cell autophagy | |||||
| Cell apoptosis | |||||
| In Vitro Model | rPNs (Rat primary neurons) | ||||
| In Vivo Model |
Rats were injected with 4 mL/kg of chloral hydrate for anesthesia and then put on a stereotactic apparatus. Subsequently, the needle was tilted at 55 in the sagittal plane and fixed anterior to the bregma (7.5 mm). The needle tip was toward the right and lowered the anterior to the chiasma (2 mm). Finally, the nonheparinized autologous femoral arterial blood (0.3 mL) was injected into a prechiasmatic cistern using a syringe pump. Rat temperature was maintained at 37 ± 0.5 during the surgery. The rats in the sham group were injected with the same dose of saline into a prechiasmatic cistern. At last, rats were monitored for recovery and then returned to cages.
Click to Show/Hide
|
||||
| Response regulation | Baicalin was confirmed to suppress the beclin1, LC3-II, and LC3-I protein levels in rat brain tissues. Moreover, we found that baicalin inhibited neuronal apoptosis. Overall, baicalin suppressed autophagy-dependent ferroptosis in early brain injury after subarachnoid hemorrhage. | ||||
Phospholipid hydroperoxide glutathione peroxidase (GPX4)
| In total 2 item(s) under this Target | |||||
| Experiment 1 Reporting the Ferroptosis-centered Drug Act on This Target | [3] | ||||
| Target for Ferroptosis | Suppressor | ||||
| Responsed Disease | Osteosarcoma | ICD-11: 2B51 | |||
| Pathway Response | Ferroptosis | hsa04216 | |||
| Cell Process | Cell ferroptosis | ||||
| In Vitro Model | MG-63 cells | Osteosarcoma | Homo sapiens | CVCL_0426 | |
| 143B cells | Osteosarcoma | Homo sapiens | CVCL_2270 | ||
| hBMMSCs (Human bone marrow mesenchymal stem cells) | |||||
| In Vivo Model |
A total of 24 BALB/c-nude mice (4-5 weeks old) were purchased and MG63 cells were injected into the right tibial bone marrow cavity of mice in a volume of 1 x 106/100 ul. When the tumor volume was visible, all animals were randomly divided into four groups (n = 6): the control (10% DMSO + 40% PEG300 + 5% Tween-80 + 45% Saline) group, the baicalin (200 mg/kg/day) group, the Fer-1 (0.8 mg/kg/day) group and Fer-1 + baicalin group. The baicalin and Fer-1 were intraperitoneally administered every day for two consecutive weeks and tumor sizes were measured every two days.
Click to Show/Hide
|
||||
| Response regulation | By promoting the Fe accumulation, ROS formation, MDA production and suppressing the ratio of GSH/GSSG, baicalin was found to trigger ferroptosis in Osteosarcoma and ferroptosis inhibitor ferrostatin-1 (Fer-1) successfully reversed these suppressive effects, indicating that ferroptosis participated in the baicalin mediated anti-OS activity. Mechanistically, baicalin physically interacted with Nrf2, a critical regulator of ferroptosis, and influenced its stability via inducing ubiquitin degradation, which suppressed the Nrf2 downstream targets GPX4 and xCT expression, and led to stimulating ferroptosis. | ||||
| Experiment 2 Reporting the Ferroptosis-centered Drug Act on This Target | [4] | ||||
| Target for Ferroptosis | Suppressor | ||||
| Responsed Disease | Intracerebral hemorrhage | ICD-11: 8B00 | |||
| Pathway Response | Fatty acid metabolism | hsa01212 | |||
| Ferroptosis | hsa04216 | ||||
| Cell Process | Cell ferroptosis | ||||
| In Vitro Model | PC12 cells | Adrenal gland pheochromocytoma | Rattus norvegicus | CVCL_0481 | |
| In Vivo Model |
A total of 60 male C57BL/6 mice (10weeks old, 25-28g) were purchased from Guangzhou University of Chinese Medicine Experimental Animal Center (Guangzhou, China). The mice were maintained with enough food and water at 24, 60% relative humidity and 12/12h light/dark cycle. The mice were randomly divided into three groups: sham operation group (Sham), ICH model group (Mod) and baicalin group (Bai) (n = 20/group). Baicalin was suspended in 0.5% carboxymethylcellulose sodium solution. Given the extremely low solubility of baicalin, the concentration of baicalin solution was 0.5 mg/ml. To achieve 20 mg/kg/day dosage, the baicalin solution was administered to the mice in the Bai group by oral route twice at an interval of 1 h within 2 h after ICH injury onset. The remaining two groups received an equal volumes of saline through oral gavage. Since the second day after ICH, mice in the Bai group received 20 mg/kg of baicalin solution while those in the remaining two groups received equal volumes of saline once a day for three consecutive days.
Click to Show/Hide
|
||||
| Response regulation | Baicalin significantly increased the mRNA expression of GPX4 and SLC7A11 in the perihematoma brain tissues of intracerebral hemorrhage (ICH) model mice. Baicalin can inhibit the development of ferroptosis in ICH. Baicalin is a potential therapeutic drug for ICH treatment. | ||||
Long-chain-fatty-acid--CoA ligase 4 (ACSL4)
| In total 1 item(s) under this Target | |||||
| Experiment 1 Reporting the Ferroptosis-centered Drug Act on This Target | [5] | ||||
| Target for Ferroptosis | Driver | ||||
| Responsed Disease | Ischemia/reperfusion injury | ICD-11: DB98 | |||
| Pathway Response | Ferroptosis | hsa04216 | |||
| Autophagy | hsa04140 | ||||
| Cell Process | Cell ferroptosis | ||||
| Cell autophagy | |||||
| In Vitro Model | CHO-S/H9C2 cells | Normal | Cricetulus griseus | CVCL_A0TS | |
| In Vivo Model |
Male Sprague-Dawley rats, 260-280 g, were provided by Beijing Vital River Laboratory Animal Technology CO., Ltd. (Beijing, China). Rats were randomly divided into five groups (n = 15 per group): control (sham operation + saline), I/R (I/R + saline), baicalin 100 mg/kg (BA-100, I/R + baicalin 100 mg/kg), baicalin 200 mg/kg (BA-200, I/R + baicalin 200 mg/kg), and diltiazem 20 mg/kg (DI-20, I/R + diltiazem 20 mg/kg). Drugs were given by oral gavage once daily (8 a.m.) for 6 days. At day 6, myocardial ischemia was induced 1 h after drug was administered.
Click to Show/Hide
|
||||
| Response regulation | Baicalin prevents against myocardial ischemia/reperfusion injury via suppressing ACSL4-controlled ferroptosis. In addition, enhanced lipid peroxidation and significant iron accumulation along with activated transferrin receptor protein 1 (TfR1) signal and nuclear receptor coactivator 4 (NCOA4)-medicated ferritinophagy were observed in in vivo and in vitro models, which were reversed by baicalin treatment. | ||||
Ferritin heavy chain (FTH1)
| In total 1 item(s) under this Target | |||||
| Experiment 1 Reporting the Ferroptosis-centered Drug Act on This Target | [6] | ||||
| Target for Ferroptosis | Marker/Suppressor | ||||
| Responsed Disease | Bladder cancer | ICD-11: 2C94 | |||
| Pathway Response | Ferroptosis | hsa04216 | |||
| Cell Process | Cell ferroptosis | ||||
| Cell proliferation | |||||
| In Vitro Model | 5637 cells | Bladder carcinoma | Homo sapiens | CVCL_0126 | |
| BLSC-KU-19 cells | Leukemia | Bos taurus | CVCL_VN09 | ||
| In Vivo Model |
All mouse experiments were approved by the Use and Care of Animals Committee at Hangzhou Normal University. About 6 x 106 KU-19-19cells were injected into the about 3-5 weeks old female BALB/c nude mice (about 18 g,n = 5).Once palpable tumors appeared, the mice were randomized in four groups: the control (deionized water containing 7% Tween 80 and 0.1% CMC-Na) group, the DFO (100 mg/kg/day) group, the baicalin (200 mg/kg/day) group, and DFO + baicalin group. After 10 days of drug administration (intraperitoneal injection, once daily), mice were sacrificed, and tumor specimens resected were collected for immunohistochemical staining and Perl's staining (Solarbio Life Sciences, G1420).
Click to Show/Hide
|
||||
| Response regulation | Baicalin triggered ferroptosis in vitro and in vivo, as evidenced by ROS accumulation and intracellular chelate iron enrichment. Baicalin exerts its anticancer activity in bladder cancer by inducing FTH1-dependent ferroptosis, which will hopefully provide great therapeutic potential for bladder cancer treatment. | ||||
Cystine/glutamate transporter (SLC7A11)
| In total 1 item(s) under this Target | |||||
| Experiment 1 Reporting the Ferroptosis-centered Drug Act on This Target | [4] | ||||
| Target for Ferroptosis | Suppressor | ||||
| Responsed Disease | Intracerebral hemorrhage | ICD-11: 8B00 | |||
| Pathway Response | Fatty acid metabolism | hsa01212 | |||
| Ferroptosis | hsa04216 | ||||
| Cell Process | Cell ferroptosis | ||||
| In Vitro Model | PC12 cells | Adrenal gland pheochromocytoma | Rattus norvegicus | CVCL_0481 | |
| In Vivo Model |
A total of 60 male C57BL/6 mice (10weeks old, 25-28g) were purchased from Guangzhou University of Chinese Medicine Experimental Animal Center (Guangzhou, China). The mice were maintained with enough food and water at 24, 60% relative humidity and 12/12h light/dark cycle. The mice were randomly divided into three groups: sham operation group (Sham), ICH model group (Mod) and baicalin group (Bai) (n = 20/group). Baicalin was suspended in 0.5% carboxymethylcellulose sodium solution. Given the extremely low solubility of baicalin, the concentration of baicalin solution was 0.5 mg/ml. To achieve 20 mg/kg/day dosage, the baicalin solution was administered to the mice in the Bai group by oral route twice at an interval of 1 h within 2 h after ICH injury onset. The remaining two groups received an equal volumes of saline through oral gavage. Since the second day after ICH, mice in the Bai group received 20 mg/kg of baicalin solution while those in the remaining two groups received equal volumes of saline once a day for three consecutive days.
Click to Show/Hide
|
||||
| Response regulation | Baicalin significantly increased the mRNA expression of GPX4 and SLC7A11 in the perihematoma brain tissues of intracerebral hemorrhage (ICH) model mice. Baicalin can inhibit the development of ferroptosis in ICH. Baicalin is a potential therapeutic drug for ICH treatment. | ||||
Beclin-1 (BECN1)
| In total 1 item(s) under this Target | |||||
| Experiment 1 Reporting the Ferroptosis-centered Drug Act on This Target | [2] | ||||
| Target for Ferroptosis | Driver | ||||
| Responsed Disease | Traumatic brain injury | ICD-11: NA07 | |||
| Pathway Response | Ferroptosis | hsa04216 | |||
| Cell Process | Cell ferroptosis | ||||
| Cell autophagy | |||||
| Cell apoptosis | |||||
| In Vitro Model | rPNs (Rat primary neurons) | ||||
| In Vivo Model |
Rats were injected with 4 mL/kg of chloral hydrate for anesthesia and then put on a stereotactic apparatus. Subsequently, the needle was tilted at 55 in the sagittal plane and fixed anterior to the bregma (7.5 mm). The needle tip was toward the right and lowered the anterior to the chiasma (2 mm). Finally, the nonheparinized autologous femoral arterial blood (0.3 mL) was injected into a prechiasmatic cistern using a syringe pump. Rat temperature was maintained at 37 ± 0.5 during the surgery. The rats in the sham group were injected with the same dose of saline into a prechiasmatic cistern. At last, rats were monitored for recovery and then returned to cages.
Click to Show/Hide
|
||||
| Response regulation | Baicalin was confirmed to suppress the beclin1, LC3-II, and LC3-I protein levels in rat brain tissues. Moreover, we found that baicalin inhibited neuronal apoptosis. Overall, baicalin suppressed autophagy-dependent ferroptosis in early brain injury after subarachnoid hemorrhage. | ||||
References
